For many, the image of medical oxygen is a steel cylinder beside a hospital bed. That cylinder represents a century of medical progress. Today, on the front lines of healthcare, from a regional hospital in Liberia to a rural clinic in Bangladesh, a technological revolution is building upon that legacy. A new generation of innovation is tackling the most persistent challenges in oxygen access: unreliable power, vast distances, and long-term maintenance.
The global health community now understands that building resilient oxygen ecosystems is fundamental to health security. The challenge is clear. A 2023 World Health Organization report noted that fewer than half of healthcare facilities in sub-Saharan Africa have access to reliable electricity. This single vulnerability can render life-saving equipment useless. The solution lies in creating a more robust, intelligent, and sustainable oxygen infrastructure, powered by new technology.
Here are three areas of innovation that are defining the future of oxygen access.
1. Unlocking Clean Power with Solar Energy
The reliability of any oxygen system is tied to its power source. In many low- and middle-income countries (LMICs), frequent power outages or voltage fluctuations from national grids pose a significant threat to patient care. Solar energy is emerging as a powerful, sustainable solution.
We are seeing remarkable progress in two main areas. First, Solar Direct-Drive Oxygen Concentrators are being designed to operate directly from solar panels without the need for batteries, which are often expensive and difficult to maintain. This simplifies the system and reduces its lifetime cost. A 2024 technical brief from PATH highlighted how these devices can deliver consistent, therapeutic oxygen flow during daylight hours, a critical capability for facilities with intermittent power.
Second, larger Solar-Powered Pressure Swing Adsorption (PSA) Plants are becoming viable for district hospitals. These systems can generate a continuous supply of medical-grade oxygen for an entire facility. By connecting PSA plants to dedicated solar arrays with battery storage, hospitals can achieve true energy independence for their oxygen production, ensuring that care never stops when the grid fails.
2. Building Smarter Systems with Better Data
Effective healthcare requires visibility. A hospital cannot manage what it cannot measure, and for years, oxygen supply has been a critical blind spot. Health workers often discovered a shortage only when a cylinder ran empty. Today, digital tools are transforming oxygen supply chains from reactive to proactive.
Innovations in remote monitoring are providing real-time data on oxygen production and consumption. Sensors attached to PSA plants, for example, can transmit performance data, purity levels, and maintenance alerts to biomedical engineers hundreds of miles away. Similarly, digital tracking systems for oxygen cylinders allow supply chain managers to monitor inventory levels across an entire region.
The Clinton Health Access Initiative (CHAI) has supported programs in several countries, including Nigeria and Ethiopia, to deploy these technologies. The data gathered allows for AI-powered demand forecasting, helping officials predict future oxygen needs with greater accuracy and prevent stockouts before they happen. This creates an intelligent network that is more efficient and reliable.
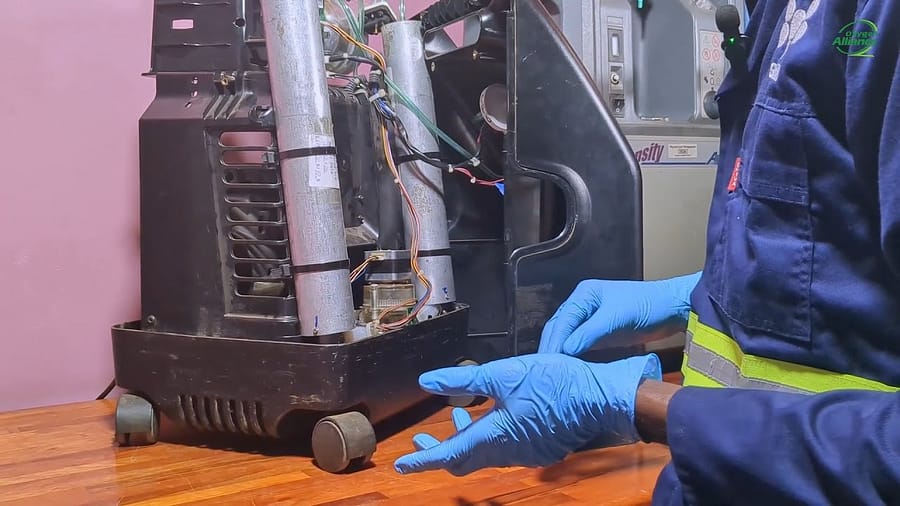
3. Designing for Sustainability and Scale
The long-term success of any technology depends on a clear plan for its upkeep. Historically, a lack of funding for maintenance and a shortage of trained technicians have been major barriers to sustainable oxygen access. A new focus on the Total Cost of Ownership (TCO) is shifting this dynamic.
Innovators and funding bodies are championing new service and business models. A 2025 call for proposals from Unitaid specifically sought innovations in sustainable service delivery. This includes pay-per-use models, where a hospital pays for the volume of oxygen it consumes, with the equipment vendor retaining responsibility for all maintenance and repairs. This approach aligns incentives and guarantees performance.
Furthermore, equipment manufacturers are increasingly designing hardware specifically for the harsh environments found in many LMICs. This involves creating devices that are more durable, require less maintenance, and use components that are easier to source and replace locally. This focus on resilient design is essential for building systems that last.
The Role of Oxygen Alliance
Oxygen Alliance operates at the intersection of this innovation and implementation. We function as a crucial bridge, connecting technology developers with the realities of health systems on the ground.
We partner with manufacturers to field-test and validate new technologies in real-world clinical settings. We gather the resulting performance data and provide it to governments and funders, helping them make evidence-based decisions about which solutions to scale. By de-risking innovation, we help accelerate its adoption and impact.
Building the Future, Together
The evolution of oxygen technology is creating a future where a patient’s access to this essential medicine is no longer dictated by an unreliable power grid or a complex supply chain. It points toward a world where oxygen access is intelligent, resilient, and universal.
We are actively seeking partners to build this future. If you are a technology developer, a medical equipment manufacturer, or a funder passionate about supporting scalable health solutions, we want to hear from you. Let’s collaborate to pilot and scale the next breakthrough in patientcare.
*References:
- Tracking SDG 7: The Energy Progress Report. World Health Organization. (2023).
- Oxygen Concentrator Technology Landscape. PATH. (2024).
- Catalyzing a Sustainable Medical Oxygen Ecosystem in Ethiopia. Clinton Health Access Initiative. (2024).
- Call for Proposals: Innovative and sustainable business models to accelerate access to medical oxygen in LMICs. Unitaid. (2025).