In the mission to advance global health, we often celebrate the arrival of new medical technologies: the MRI machine, the ventilator, the infant incubator. We must also consider what happens after the ribbon-cutting ceremony. The shocking reality is that in many low- and middle-income countries (LMICs), a staggering percentage of this vital equipment, in some regions as high as 50%, is out of service. This is a systemic failure, resulting in cancelled procedures, delayed diagnoses, and preventable deaths. As our foundational webinar, “Introduction to Medical Equipment Management,” revealed, the solution requires a smarter, more strategic approach to the entire life cycle of medical technology.
Why We Get It Wrong: The Fallacy of “Donate and Disappear”
The problem is deeply rooted in a broken paradigm. A study in Uganda found that on average, 34% of medical equipment in health facilities was faulty, and a shocking 85.6% of devices lacked a user manual. This points to a systemic failure that begins long before a device breaks down. Our webinar identified several key missteps:
- Procurement without a Plan: Equipment is often acquired without a thorough needs assessment or consideration for the local context. Factors include the stability of the power grid, environmental conditions, or the availability of trained technicians and spare parts.
- The Missing Link of Training: A device is only as good as the person operating it. Training for both clinical users and technical staff is frequently an afterthought, leading to improper use and avoidable damage.
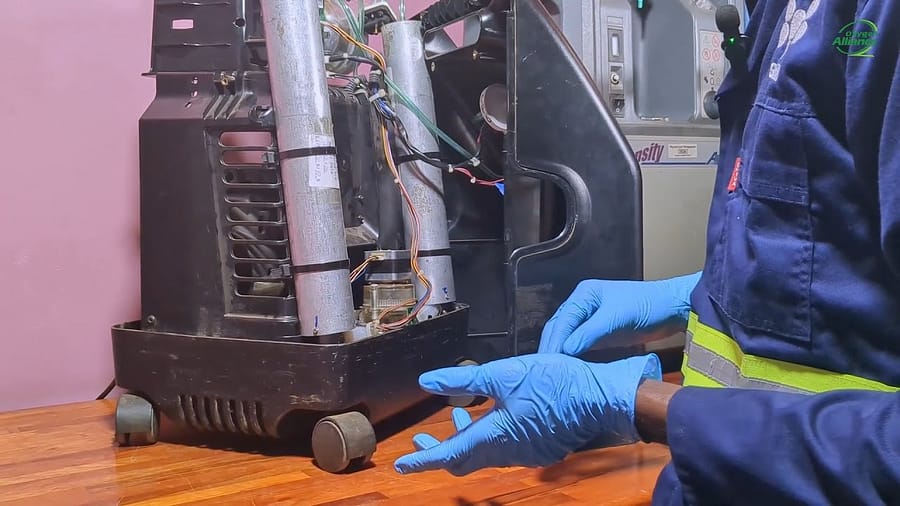
- Reactive vs. Proactive Maintenance: The dominant model is one of “corrective maintenance,” which means waiting for a device to fail before acting. This is incredibly inefficient and costly compared to a “preventive” approach that identifies and addresses issues before they lead to a breakdown.
The economic impact is immense. One analysis revealed that for every $10 cut from operational maintenance, hospitals can face up to $40 in additional capital expenses down the line. For resource-constrained health systems in LMICs, this is a devastating financial blow.
A Life-Cycle Approach
The core message of our webinar was a call for a fundamental shift in perspective. We must manage medical equipment as a long-term asset across its entire life cycle. This involves:
- Meticulous Planning & Procurement: Conducting a rigorous needs assessment and developing clear technical specifications before any purchase is made.
- Robust Commissioning: Ensuring that upon arrival, equipment is properly installed, calibrated, and that staff are thoroughly trained on its operation and routine care.
- Systematic Inventory & Maintenance: Creating a comprehensive inventory of all medical devices is the bedrock of good management. This allows for the development of a planned preventive maintenance (PPM) schedule, ensuring that every piece of equipment is regularly inspected, serviced, and calibrated.
- Responsible Decommissioning: Safely and ethically disposing of equipment at the end of its life, in accordance with local regulations, and salvaging usable parts to support other devices.
Building Systems, Not Stockpiles
The challenge of non-functional medical equipment is one of the most significant, yet solvable, obstacles to achieving health equity. The solution is a more intelligent and sustainable system for managing technology. By investing in training, championing preventive maintenance, and adopting a strategic life-cycle approach, we can dramatically increase the uptime of these life-saving tools. This is how we honor the investment of our donors, empower our partners on the front lines, and ensure that every patient has access to the quality care they deserve.
To learn the fundamentals of building a robust medical equipment management system, watch our introductory webinar